What is HCM?
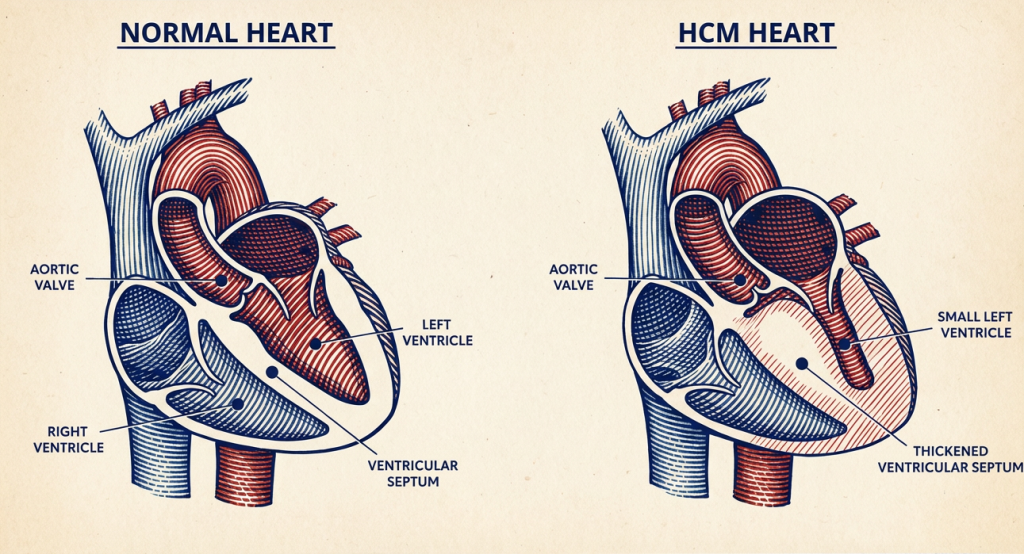
Hypertrophic cardiomyopathy (HCM) is the most common heart disease in cats. It happens when the heart muscle—usually the left ventricle—becomes abnormally thickened.
When the muscle thickens, the heart can’t relax and fill properly between beats. This can:
- Reduce how efficiently the heart pumps blood
- Increase pressure inside the heart
- Cause the left atrium to enlarge
- Lead to fluid build-up (heart failure) or blood clots
Some cats live for years with mild HCM and no outward signs; others can develop serious complications.
What causes HCM in cats?
In many cats, the exact cause isn’t identified, but HCM is often thought to have a genetic component, especially in certain breeds.
HCM can be:
- Primary (idiopathic/genetic) – most common
- Secondary changes – heart muscle thickening can occur due to other conditions that increase heart workload (such as high blood pressure or hyperthyroidism); these changes may resemble HCM, and your vet will check for underlying causes
Important: HCM is not caused by being “too active”. Activity doesn’t create HCM; however, symptoms may become more noticeable when the heart is struggling.
Which cats are most at risk?
Any cat can develop HCM, but risk is higher in:
- Cats with a close relative diagnosed with HCM
- Middle-aged to older cats (though it can occur in younger cats too)
Prevalence estimate: HCM may affect as many as ~1 in 7 cats, though figures vary by study and population.
Signs of HCM to watch out for
Many cats show no signs until disease is advanced, which is why routine checks matter.
Possible signs include:
- Faster or more effortful breathing
- Lethargy / hiding more than usual
- Reduced appetite or weight loss
- Weakness or collapse
- Heart murmur or abnormal rhythm found at a check-up (not all cats with HCM have a murmur)
Emergency red flags (get urgent veterinary help)
- Open-mouth breathing, severe breathlessness, or rapid breathing at rest
- Sudden hind-leg weakness/paralysis with pain (can indicate an arterial blood clot, often called a “saddle thrombus”)
- Collapse or severe distress
How is HCM diagnosed?
A vet may suspect heart disease from a murmur, gallop sound, arrhythmia, or symptoms—but the best test to confirm HCM is:
- Echocardiography (heart ultrasound) – this measures wall thickness and heart function
Note: Not all cats with HCM have a murmur — an echo is the definitive test.
Other tests often used to assess severity and look for underlying contributors:
- Chest x-rays (if heart failure suspected)
- Blood pressure
- Thyroid testing (especially in older cats)
- Electrocardiogram (ECG)
- Sometimes cardiac biomarkers
Treatment: what can be done?
There is no cure that reverses genetic HCM in cats, but treatment can:
- control symptoms
- reduce complication risk
- improve quality of life
Treatment depends on stage/severity:
If a cat has no symptoms yet: Some cats are monitored without medication, especially if changes are mild. Your vet/cardiologist will advise follow-up intervals.
If heart failure develops: Medications may be used to manage fluid build-up and support function (your vet will tailor these to the cat’s exact findings).
If clot risk is high: Blood clots are one of the most serious complications. Clopidogrel is specifically highlighted in veterinary references as reducing the incidence of arterial thromboembolism in cats.
Do not start/stop heart meds without your vet. The “right” meds differ depending on whether obstruction is present, whether there’s heart failure, clot risk, blood pressure, and other conditions.
Can HCM be prevented?
In most pet cats, HCM cannot be fully prevented. It is often genetic or idiopathic, meaning there is no guaranteed way to stop it from developing in an individual cat.
Reducing risk and improving outcomes
While HCM can’t always be prevented, there are proven ways to reduce risk, detect it earlier, and improve quality of life:
Choose a responsibly bred kitten
- If buying a Bengal, Maine Coon, Ragdoll, or another breed where screening is common, ask whether breeding cats have had cardiologist-performed echocardiograms, whether screening is repeated, and whether affected cats are removed from breeding programmes.
(This does not guarantee prevention, but it reduces risk at a population level.)
Maintain a healthy body weight
- Obesity does not cause HCM, but it increases cardiovascular strain and can worsen outcomes.
Attend routine veterinary check-ups
- Many cats show no early signs. If a murmur or abnormal rhythm is detected, ask whether referral for an echocardiogram is appropriate.
Manage conditions that increase heart workload
- High blood pressure and hyperthyroidism (especially in older cats) can worsen heart disease and should be treated if present.
Monitor breathing at rest when advised
- For cats with known heart disease or suspected risk, monitoring sleeping respiratory rate can help detect fluid build-up early. Ask your vet what’s normal for your cat.
Living With a Cat Who Has HCM
Many cats with HCM live good-quality lives with:
- appropriate medication (if needed)
- regular monitoring
- a calm, stable routine
- prompt action if breathing or mobility changes
Prognosis varies widely and is poorer once congestive heart failure or blood clots develop.
When to Seek Urgent Veterinary Care
Get immediate veterinary help if your cat shows:
- Collapse, fainting, or sudden weakness (such as falling over or being unable to stand)
- Breathing distress or open-mouth breathing
- Sudden painful hind-leg weakness or paralysis
- Severe lethargy with rapid breathing
Quick FAQs
“My cat has a heart murmur — does that mean HCM?”
Not always. Some murmurs are harmless, and some cats with HCM have no murmur. An echocardiogram is the most reliable way to diagnose HCM.
“Can diet or supplements prevent HCM?”
No supplements are proven to prevent genetic HCM. The most effective measures are responsible breeding, maintaining a healthy weight, and early detection.
Sources
- https://vcahospitals.com/know-your-pet/hypertrophic-cardiomyopathy-in-cats
- https://www.petmd.com/cat/conditions/cardiovascular/c_ct_hypertrophic_cardiomyopathy
- https://www.cats.org.uk/help-and-advice/health/heart-disease
- https://www.cornell.edu/hcm-cats
- https://www.fabcats.org/cat-care/health-advice/heart-disease/